A venous
plasma glucose concentration below 50 mg/dl is called hypoglycaemia. The
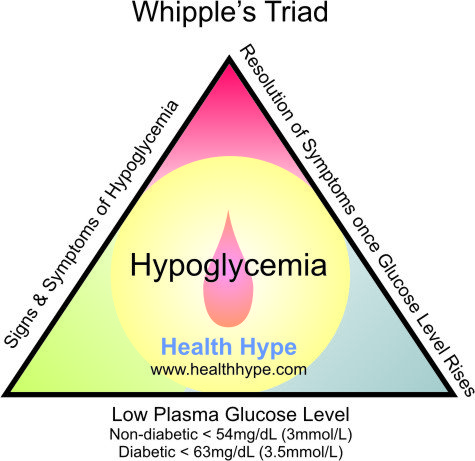
diagnosis of hypoglycemia necessitates the presence of Whipple’s triad. This
consists of:
The classic
signs and symptoms of hypoglycemia are trembling, sweating, nausea, rapid
pulse, lightheadedness, hunger and epigastric discomfort. Neuroglycopenia can
be seen in severe cases (headache, confusion, blurred vision, dizziness, and
seizures).
REGULATORY RESPONSE TO HYPOGLYCEMIA
ACTIVATION OF PARASYMPATHETIC NERVOUS SYSTEM
DEMONSTRAITON OF HYPOGLYCEMIA
PROVOCATION TEST:
Mixed meal test:
2) Low
plasma glucose concentration and
3) Symptoms
relieved by glucose administration.
 |
| Fig. Classical Signs and symptoms of Hypoglycemia |
The most
common cause of hypoglycemia are drugs like propranolol, salicylate, oral
hypoglycemic drugs with long half life like chlorpropamide, insulin secreting
sulfonylureas, glycogen storage disease, alcoholism, septicemia, hepatic
failure, Addison’s disease etc.
REGULATORY RESPONSE TO HYPOGLYCEMIA
In
hypoglycemia, the shortage of glucose in neurons activates hypothalamus, and an
autonomic response to restore and maintain glucose supply initiates which has
many effects like:
ACTIVATION OF SYMPATHETIC NERVOUS SYSTEM
α-ADRENERGIC EFFECTS
- Inhibition of endogenous insulin release
- Increased cerebral blood flow (peripheral vasoconstriction)
β-ADRENERGIC EFFECTS:
- Stimulation of glycogenolysis
- Stimulation of glucagon release (also α cells can sense directly)
- Stimulation of lipolysis
- Inhibition of muscle glucose uptake
- Increased cerebral blood flow (by increasing cardiac output)
CATECHOLAMINE RELEASE FROM ADRENAL MEDULLA
- Potentiates the α and β adrenergic effects
ACTIVATION OF PARASYMPATHETIC NERVOUS SYSTEM
- Stimulates vagus nerve
- Stimulation of gastric acid secretion
- Stimulation of parotid salivary secretion.
There is
hierarchy of response of counter-regulatory hormones; glucagon, epinephrine,
cortisol and GH. Glucagon and epinephrine are rapidly acting hormones whereas
latter two are slow acting and are active at late phase of hypoglycemia. During
fast state the first mechanism is inhibition of endogenous insulin secretion
and followed by release of counter regulatory hormones in hierarchy.
Decreased
endogenous insulin occurs at glucose level 80 mg/dl; increase glucagon,
adrenaline, cortisol and GH secretion at 60 mg/dl and development of
hypoglycaemic symptoms occurs at 50 mg/dl and impairment of cognitive function
at 40 mg/dl.
INVESTIGATION OF HYPOGLYCEMIA
First is
demonstration of hypoglycemia and second to identify the cause of hypoglycemia.
DEMONSTRAITON OF HYPOGLYCEMIA
MEASUREMENT OF BLOOD GLUCOSE
Measurement
of blood glucose (insulin, C-peptide) during acute neuroglycopenia
(characterized by sweating, anxiety, hunger, palpitation and weakness) is the
best test for the diagnosis of hypoglycemia.
PROVOCATION TEST:
Prolonged fast:
This is the
single most useful test to evaluate suspected hypoglycemia. The aim of this
test is to demonstrate spontaneous hypoglycemia in the presence of
neuroglycopenic symptoms during prolonged fasting for 48 h, and that the
symptoms resolve on glucose administration.
During the
fasting period blood glucose, insulin, C-peptide is measured at every 4-6
hours. But as glucose level falls below 50 mg/dl frequent sample must be taken.
About 95% of patient will develop hypoglycaemia within 48 h. Measurement of
β-hydroxybutyrate and its raising presence indicates suppression of insulin release
and fast can be terminated by giving glucose when FBS becomes <45 mg/dL and
patient exhibit signs or symptoms of hypoglycemia.
Mixed meal test:
This is used
to investigate patients who experience postprandial symptoms, for the
possibility of reactive hypoglycemia. Meal is ingested and plasma glucose
measured every 30 min for 6h and at any time during symptomatic phase. Patients
developing neuroglycopenia symptoms during hypoglycemia, but not at other times
during the test, are considered to have postprandial hypoglycemia.


No comments:
Post a Comment