Formerly called Insulin dependent diabetes mellitus (IDDM). Accounts for about
5-10% of diabetes. Occurs due to beta
cell destruction leading to absolute insulin deficiency, so that patient
requires exogenous supply of insulin. It is characterized by hyperglycemia
severe cachexia (if untreated), dehydration and ketoacidosis. It is apparent
within week or month, i.e., early and abrupt onset of symptoms in childhood and
adolescence (polyuria, polydipsia and weight loss). About 75% acquire the
disease and are diagnosed before 30 years of age but in remainder can occur in
any age.
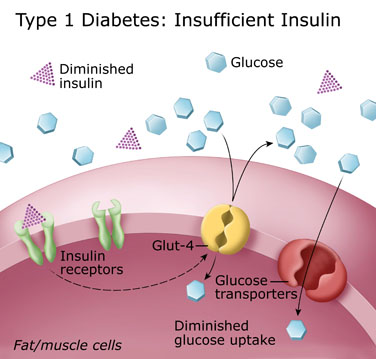 |
| Fig. Type 1 Diabetes mechanism |
LADA is rare subtype of type 1 diabetes. Individual develop diabetes
insidiously and respond initially to treatments other than insulin, like
sulphonylureas. Some patients with autoimmune type 1 diabetes although have
ketoacidosis, but has sufficient islet cells reserve for some months after the
diagnosis to remain ketosis free on little or even no insulin (so called
honeymoon period). Some patients with type 2 diabetes may become ketosis prone
as beta cell failure progresses from being relative to being absolute due to
islet cell exhaustion or destruction, particularly in conditions of increased
insulin requirement such as systemic sepsis. The acceleratory hypothesis of
type 2 diabetes predisposing to type 1 diabetes via islet cell stress and high
prevalence of co-aggregation of features of both types of diabetes is called
double diabetes effect. Some patients
have no evidence of autoimmunity and are classified as type 1 idiopathic.
For the confirmation of type 1 (autoimmune) diabetes quantification of
anti-glutamic acid decarboxylase (GAD) antibodies and/or islet cell antibodies
(ICA) may be helpful. These antibodies are also present in 2% of normal
individuals. But in individuals with these antibodies are at increased risk of
diabetes.
AETIOLOGY
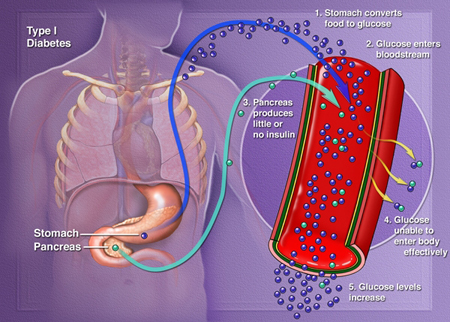 |
| Fig. Cause of Type 1 Diabetes |
Type 1 diabetes results from autoimmune (CMI, mostly T cell) attack of
pancreatic β cells.
Many factors are associated with this dysfunction. The islet cells have a
chronic mononuclear cell infiltrate, called insulitis. The autoimmune process
begins months or years before clinical presentation, and an 80% to 90%
reduction in the volume of beta cell is required to induce symptoms. The
process of β
cell destruction takes many months and occurs in cycles of deterioration and
remission. The remission period with normal β cell function is called honeymoon
period and it lasts for 6 month upto 24 months. Although the main defect is
autoimmune destruction of β cells but insulin resistance also develops due to
formation of anti insulin antibodies and other mechanisms like obesity.
ANTIBODIES
The most
practical markers of beta cell autoimmunity are circulating antibodies that can
be detected in serum years before the onset of hyperglycemia. The best
characterized antibodies are;
- Islet cell cytoplasmic antibodies (ICA): These reacts with a sialoglycoconjugate antigen present in the cytoplasm of all endocrine cells of the pancreatic islets. These are seen in some normal persons but occur in 75-85% of T-1 diabetics.
- Insulin autoantibodies (IAAs): High titer IAAs are present in children who develop T-1 diabetes, >90% of children <5 years with diabetes has IAA. IAA can develop even in human insulin therapy. IAA also occurs in very few normal individuals.
- Antibodies to the 65-kD isoform of glutamic acid decarboxylase (GAD65): These are found up to 10 years before the onset of type 1 diabetes and present in most of newly diagnosed diabetics. These antibodies can be used to determine the likelihood of conversion of type 2 to type 1.
- Insulinoma-associated antibodies (IA-2A and IA-2βA): These antibodies are directed against two tyrosine phosphatases, are present in more than 50% of diabetics.
- Autoantibody markers of immune destruction are present in 85% to 90% of immune mediated diabetics when fasting hyperglycemia is detected. Some individuals with type 2 diabetes phenotype also have ICA, particularly GAD65A. This condition has been termed Latent autoimmune diabetes of adulthood (LADA). The presence of multiple autoantibodies is associated with >90% risk of immune mediated diabetes.
Environmental factors are also
involved in initiating diabetes. Viruses like rubella, mumps, etc. have been
implicated. Other factors suggested are chemicals and cow’s milk.

You made some decent points there. I looked on the internet for the issue and found most individuals will go along with your opinion. Thanks!Sigma antibody
ReplyDelete